How to resolve pharmacy insurance rejections information
Home » Trending » How to resolve pharmacy insurance rejections informationYour How to resolve pharmacy insurance rejections images are ready. How to resolve pharmacy insurance rejections are a topic that is being searched for and liked by netizens now. You can Get the How to resolve pharmacy insurance rejections files here. Download all free photos and vectors.
If you’re looking for how to resolve pharmacy insurance rejections images information linked to the how to resolve pharmacy insurance rejections interest, you have visit the ideal blog. Our website always provides you with hints for downloading the maximum quality video and image content, please kindly hunt and locate more enlightening video articles and graphics that match your interests.
How To Resolve Pharmacy Insurance Rejections. No letters in enrolee id. Now denials are becoming a big catastrophe for many health systems and hospitals. Bragdon estimates that 10 percent of total new prescriptions require a prior authorization, and there’s usually a jump at the new year and when patients switch insurance. Claim denials can often be resolved over the phone, but you can also submit an appeal in writing.
 How to Save Money on Prescription Medication From savingadvice.com
How to Save Money on Prescription Medication From savingadvice.com
1 identify the path of a prescription insurance claim after it leaves the pharmacy 2 recognize common rejections, what they mean, and when and how they should be overridden 3 identify key elements of the revenue cycle of a pharmacy, from submission to final payment If you are calling from the pharmacy, please dial 1‑844‑233‑8244. I�ve had almost no help from staff other than them randomly mentioning one here or there. Our average wait time is about 1 minute. • pharmacies enter into an agreement /c ontract with a pbm and a rate/formula is set for dispensing brands, generics, and specialty medications Pharmacy reimbursement is the “behind the scenes” component of processing a patients prescription.
No letters in enrolee id.
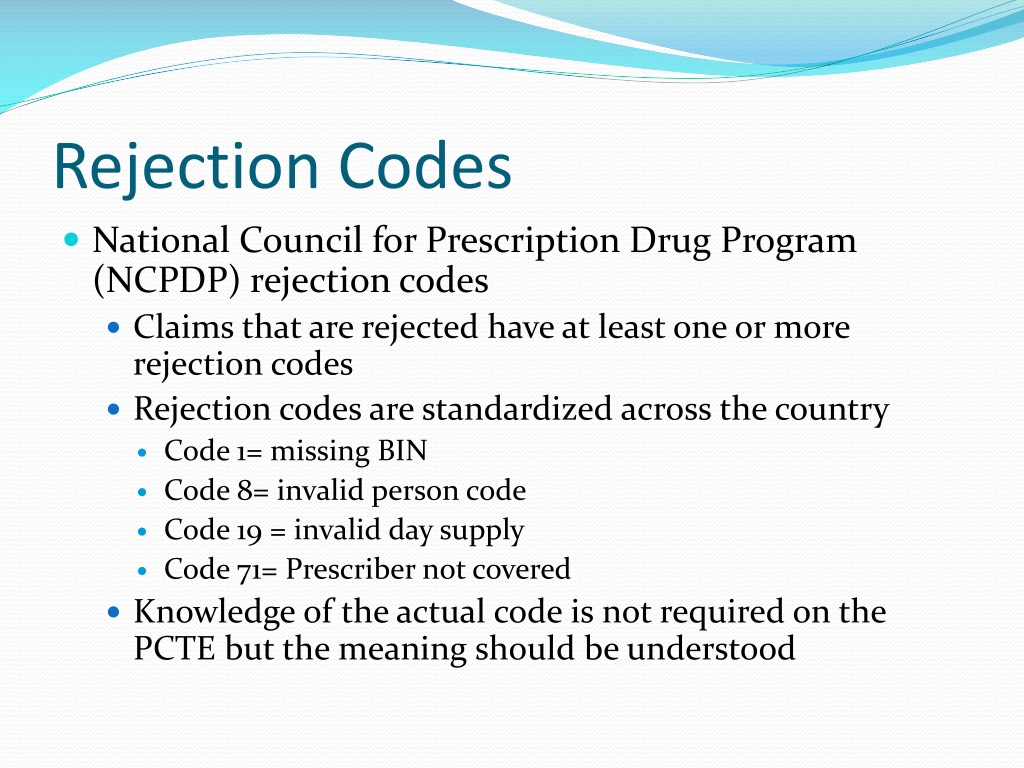
Sometimes these issues can be solved by calling the insurance company, but depending upon volume of customers and staff, a call to the insurance company (and subsequently getting put on hold by the insurance company), which also may or may not also require a call to the doctor’s office, will put a kink in your productivity. Case scenarios issues related to insurance rejections are potentially some of the most complex circumstances we can encounter in the pharmacy setting. Train billing staff to handle rejections quickly and provide training on how to appropriately handle denials. And the process varies considerably among prescribers and insurance, with resolution coming in as little as one hour to as much as several weeks, he said. Pharmacy ncpdp reject codes last updated 10/2021 ncpdp reject code ncpdp reject code description interchange edit description 6c m/i other payer id qualifier 0882 other payer id qualifier not applicable 6e m/i other payer reject code. If it is a control, its store/dea regulations will only allow us to release this medication on x date.
 Source: savingadvice.com
Source: savingadvice.com
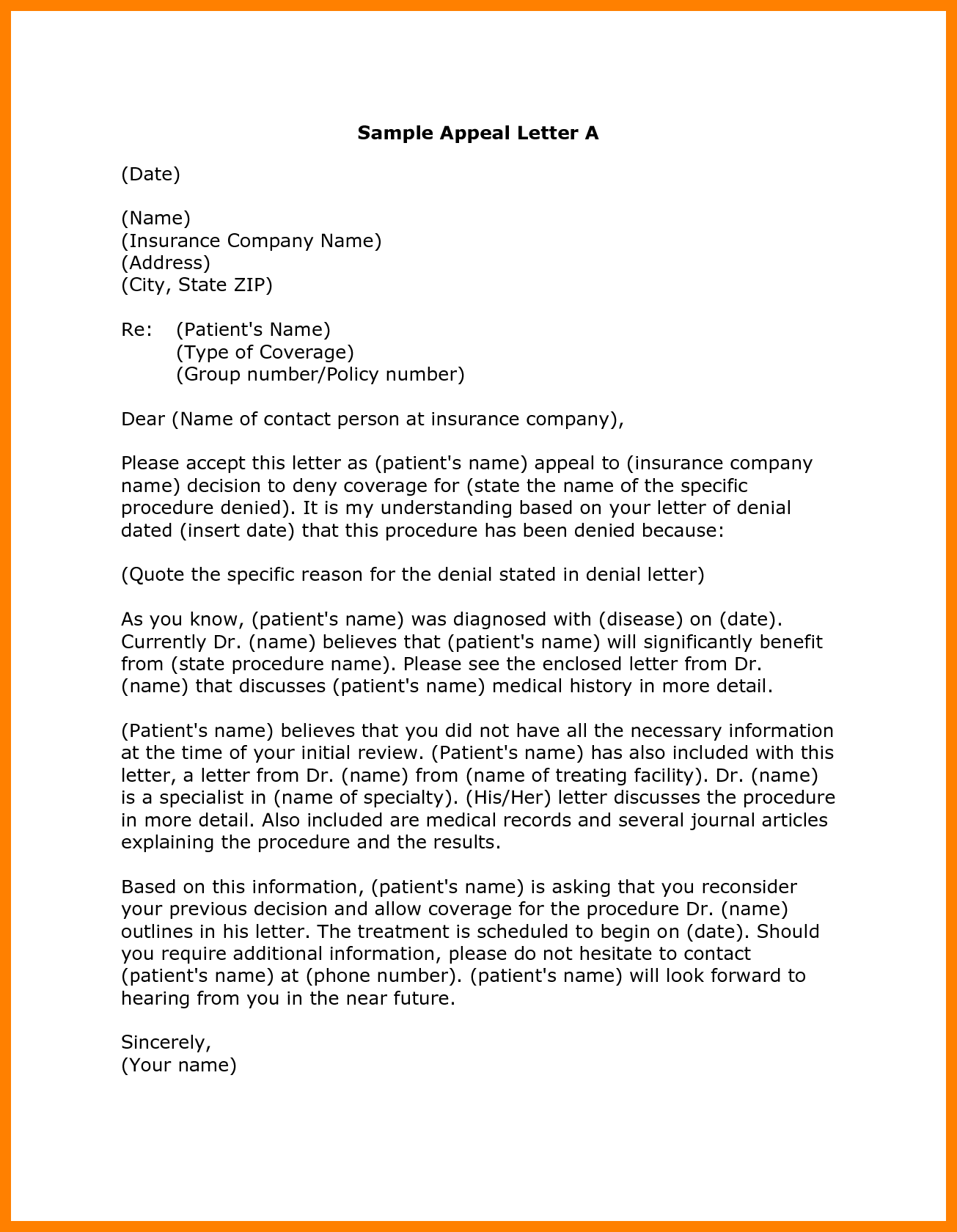
So, the finest way to escape from rejections and denials is to submit “clean claims”. Unbelievably there is no training on this and no central list, so here�s what i�ve compiled (it�s probably half wrong). Drug rejection by an insurance company ; So, the finest way to escape from rejections and denials is to submit “clean claims”. Claim denials can often be resolved over the phone, but you can also submit an appeal in writing.
 Source: slideserve.com
Source: slideserve.com
Rejections such as refill too soon, prior authorization, and drug not covered are common rejections encountered in pharmacies each day. 1 identify the path of a prescription insurance claim after it leaves the pharmacy 2 recognize common rejections, what they mean, and when and how they should be overridden 3 identify key elements of the revenue cycle of a pharmacy, from submission to final payment Let’s explore some of the ways pharmacies get reimbursed…. 1.) read the reject and try to decipher it: We will help you resolve your issue as quickly as possible.
 Source: theleaderpharm.com
Source: theleaderpharm.com
Train billing staff to handle rejections quickly and provide training on how to appropriately handle denials. 1 identify the path of a prescription insurance claim after it leaves the pharmacy 2 recognize common rejections, what they mean, and when and how they should be overridden 3 identify key elements of the revenue cycle of a pharmacy, from submission to final payment With insurance rejections, put the onus on the insurance not you or the customer. As mentioned in the dx and nr rejections above, the dx field indicates the patient�s copay amount left over from the primary claim. • service appropriate to bill.
 Source: pharmacy-tech-resources.com
Source: pharmacy-tech-resources.com
Tips to avoid duplicate rejections or denials • always check the status of a claim before resending. Similar to the copay amount qualifier rejection above. So, the finest way to escape from rejections and denials is to submit “clean claims”. Bragdon estimates that 10 percent of total new prescriptions require a prior authorization, and there’s usually a jump at the new year and when patients switch insurance. Schedule routine chart audits for data and documentation quality to identify problems and trends before claims are sent to the payer.
 Source: naponewsonline.org
Source: naponewsonline.org
Pharmacy reimbursement is the “behind the scenes” component of processing a patients prescription. Now denials are becoming a big catastrophe for many health systems and hospitals. Group # not working try mibcnrx1. The more experience you have with billing prescriptions, the easier it will be for you to recognize the rejections and resolve them. Therefore, healthcare providers need to accomplish all definite standards of health insurance companies to.
 Source: mthomearts.com
Source: mthomearts.com
Group # not working try mibcnrx1. Because it will cost health systems up to 2% of their net revenue. Let’s explore some of the ways pharmacies get reimbursed…. Can improve profitability with insurance and reduce liability pharmacy technician. If it is a control, its store/dea regulations will only allow us to release this medication on x date.
 Source: slideserve.com
Source: slideserve.com
If you come across a rejection you are not familiar with, contact the insurance company for clarification. • verify initial denial reason. Rejections such as refill too soon, prior authorization, and drug not covered are common rejections encountered in pharmacies each day. Schedule routine chart audits for data and documentation quality to identify problems and trends before claims are sent to the payer. The insurance company’s address and policy number if your claim has already been rejected or denied because of a data entry mistake, you can always call the insurer and ask for reconsideration.
 Source: blog.bcbsnc.com
Source: blog.bcbsnc.com
Group # not working try mibcnrx1. We will help you resolve your issue as quickly as possible. • sometimes the pharmacist will enter diagnosis codes in the patient file (f3) , and they will wonder why the insurance company is not receiving the codes in the transmission. And the process varies considerably among prescribers and insurance, with resolution coming in as little as one hour to as much as several weeks, he said. I�ve had almost no help from staff other than them randomly mentioning one here or there.
 Source: pharmacy-tech-resources.com
Source: pharmacy-tech-resources.com
Sometimes these issues can be solved by calling the insurance company, but depending upon volume of customers and staff, a call to the insurance company (and subsequently getting put on hold by the insurance company), which also may or may not also require a call to the doctor’s office, will put a kink in your productivity. The more experience you have with billing prescriptions, the easier it will be for you to recognize the rejections and resolve them. Our average wait time is about 1 minute. We also answer additional questions in our faqs from pharmacy staff. As mentioned in the dx and nr rejections above, the dx field indicates the patient�s copay amount left over from the primary claim.
 Source: medbillingexperts.com
Source: medbillingexperts.com
1.) read the reject and try to decipher it: Sometimes these issues can be solved by calling the insurance company, but depending upon volume of customers and staff, a call to the insurance company (and subsequently getting put on hold by the insurance company), which also may or may not also require a call to the doctor’s office, will put a kink in your productivity. So, the finest way to escape from rejections and denials is to submit “clean claims”. Rejections such as refill too soon, prior authorization, and drug not covered are common rejections encountered in pharmacies each day. We also answer additional questions in our faqs from pharmacy staff.
 Source: blog.computer-rx.com
Source: blog.computer-rx.com
• submit an appeal for denied claims, providing documentation with redetermination request. Rejections such as refill too soon, prior authorization, and drug not covered are common rejections encountered in pharmacies each day. To correct it, pull up the secondary insurance company in the vendor file maintenance, type �o3� to go to screen three, and add /opa to line 16. If you come across a rejection you are not familiar with, contact the insurance company for clarification. This time of the year sucks, everyone�s stupid insurance expired and they claim nothing has changed there is no book.and i think the rejects possibly vary per state.
 Source: guidelineshealth.com
Source: guidelineshealth.com
Let’s explore some of the ways pharmacies get reimbursed…. This prescription may be able to be overridden with some override codes at the pharmacy.) Drug rejection by an insurance company ; Tips to avoid duplicate rejections or denials • always check the status of a claim before resending. Can improve profitability with insurance and reduce liability pharmacy technician.
 Source: m-scribe.com
Source: m-scribe.com
The insurance company’s address and policy number if your claim has already been rejected or denied because of a data entry mistake, you can always call the insurer and ask for reconsideration. Rejections such as refill too soon, prior authorization, and drug not covered are common rejections encountered in pharmacies each day. If you come across a rejection you are not familiar with, contact the insurance company for clarification. The insurance company’s address and policy number if your claim has already been rejected or denied because of a data entry mistake, you can always call the insurer and ask for reconsideration. Train billing staff to handle rejections quickly and provide training on how to appropriately handle denials.
 Source: template.net
Source: template.net
Claims rejections are claims that fail to meet specific criteria and data requirements that are rejected by insurance companies. This time of the year sucks, everyone�s stupid insurance expired and they claim nothing has changed there is no book.and i think the rejects possibly vary per state. Let’s explore some of the ways pharmacies get reimbursed…. And the process varies considerably among prescribers and insurance, with resolution coming in as little as one hour to as much as several weeks, he said. • if an insurance company is expecting a certain diagnosis code and the pharmacist puts a different diagnosis code there or doesn’t put one in at all, the claim will be rejected.
 Source: pcisgold.com
Now denials are becoming a big catastrophe for many health systems and hospitals. To correct it, pull up the secondary insurance company in the vendor file maintenance, type �o3� to go to screen three, and add /opa to line 16. Because it will cost health systems up to 2% of their net revenue. If you are calling from the pharmacy, please dial 1‑844‑233‑8244. If it is a control, its store/dea regulations will only allow us to release this medication on x date.
 Source: atlanticrcm.com
Source: atlanticrcm.com
Sometimes these issues can be solved by calling the insurance company, but depending upon volume of customers and staff, a call to the insurance company (and subsequently getting put on hold by the insurance company), which also may or may not also require a call to the doctor’s office, will put a kink in your productivity. • sometimes the pharmacist will enter diagnosis codes in the patient file (f3) , and they will wonder why the insurance company is not receiving the codes in the transmission. Rejections such as refill too soon, prior authorization, and drug not covered are common rejections encountered in pharmacies each day. This time of the year sucks, everyone�s stupid insurance expired and they claim nothing has changed there is no book.and i think the rejects possibly vary per state. Pharmacy ncpdp reject codes last updated 10/2021 ncpdp reject code ncpdp reject code description interchange edit description 6c m/i other payer id qualifier 0882 other payer id qualifier not applicable 6e m/i other payer reject code.
 Source: pinterest.com
Source: pinterest.com
If you come across a rejection you are not familiar with, contact the insurance company for clarification. The insurance company’s address and policy number if your claim has already been rejected or denied because of a data entry mistake, you can always call the insurer and ask for reconsideration. Pharmacy reimbursement is the “behind the scenes” component of processing a patients prescription. We will help you resolve your issue as quickly as possible. 1 identify the path of a prescription insurance claim after it leaves the pharmacy 2 recognize common rejections, what they mean, and when and how they should be overridden 3 identify key elements of the revenue cycle of a pharmacy, from submission to final payment
 Source: myprepexperience.blogspot.com
Source: myprepexperience.blogspot.com
• submit an appeal for denied claims, providing documentation with redetermination request. • service appropriate to bill. We also answer additional questions in our faqs from pharmacy staff. Rejections such as refill too soon, prior authorization, and drug not covered are common rejections encountered in pharmacies each day. The pharmacist should deal with insurance issues by communicating first with the patient, then with the prescriber, and.
This site is an open community for users to do submittion their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site helpful, please support us by sharing this posts to your preference social media accounts like Facebook, Instagram and so on or you can also bookmark this blog page with the title how to resolve pharmacy insurance rejections by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.
