Insurance authorization specialist Idea
Home » Trending » Insurance authorization specialist IdeaYour Insurance authorization specialist images are available. Insurance authorization specialist are a topic that is being searched for and liked by netizens now. You can Get the Insurance authorization specialist files here. Get all royalty-free photos and vectors.
If you’re searching for insurance authorization specialist pictures information related to the insurance authorization specialist topic, you have pay a visit to the ideal blog. Our website frequently gives you suggestions for viewing the maximum quality video and image content, please kindly hunt and locate more enlightening video content and graphics that fit your interests.
Insurance Authorization Specialist. Apply for the job in insurance authorization specialist at ridgefield, ct. The insurance authorization specialist is responsible for selecting accurate medical records for patient safety and working with insurance companies and/or physician offices to complete insurance authorization requirements to secure payment. The national average salary for an insurance authorization specialist is $43,587 per year in united states. Serves as a patient advocate and functions as a liaison between the patient and payor to address reimbursement questions and avoid insurance delays.
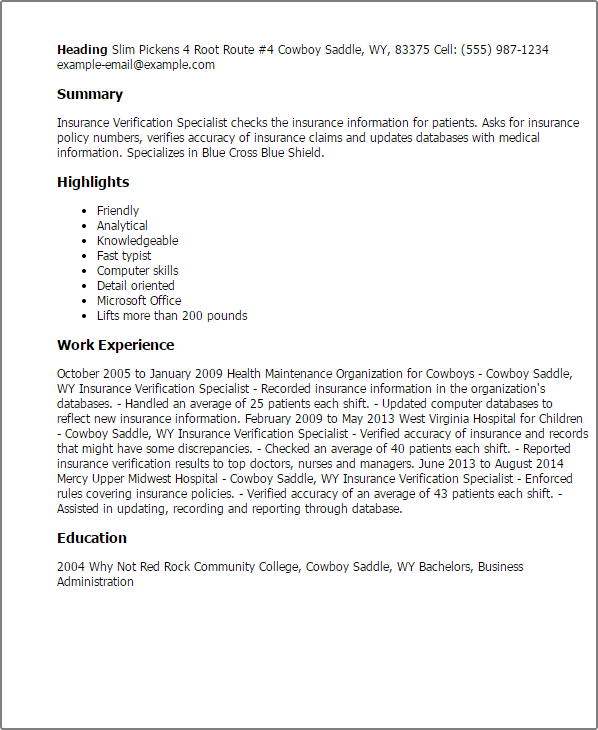
 Insurance Referral & Authorization Manager Resume Example From livecareer.com
Insurance Referral & Authorization Manager Resume Example From livecareer.com
Lehigh valley health network allentown, pa. Serves as a patient advocate and functions as a liaison between the patient and payor to address reimbursement questions and avoid insurance delays. Insurance authorization specialist responsibilities include: They interview patients to assess their needs and work with insurance companies and. Apply for the job in insurance authorization specialist at ridgefield, ct. Actually the specialists have shifted to the authorization wing of the insurance company where the doctors refer for authorization before starting any procedure on the insured patient.
Health care and home care experience preferred.
Knowledge of medical terminology is. Many of the low premium insurance covered patients suffer in the hands of the specialist’s ingenious ways to deny the permission for procedure. Get more data about insurance authorization. Apply to authorization specialist, insurance verification specialist, prior authorization specialist and more! Salaries estimates are based on 18 salaries submitted anonymously to glassdoor by an insurance authorization specialist employees. Obtains authorizations for surgical procedures, diagnostic testing, medications, outgoing referrals, and other services as part of daily operations.
 Source: qwikresume.com
Source: qwikresume.com
Apply to insurance verification specialist, prior authorization specialist, authorization specialist and more! Authorization specialists file documents and gather the required information for. The authorization specialist job role is to take insurance information from the clients and determine if any authorization is required for the service that is to be undertaken. Serves as a patient advocate and functions as a liaison between the patient and payor to address reimbursement questions and avoid insurance delays. Knowledge of third party payer regulations including medicare, minnesota medical assistance, veterans affairs (va) and private insurance.
 Source: livecareer.com
Source: livecareer.com
Get more data about insurance authorization. You will evaluate portions to be paid by the customer as well as perform all insurance related assignments as instructed. The authorization specialist job role is to take insurance information from the clients and determine if any authorization is required for the service that is to be undertaken. Insurance authorization specialist job description template. The insurance authorization specialist is responsible for selecting accurate medical records for patient safety and working with insurance companies and/or physician offices to complete insurance authorization requirements to secure payment.
 Source: priorauthtraining.org
Source: priorauthtraining.org
Many of the low premium insurance covered patients suffer in the hands of the specialist’s ingenious ways to deny the permission for procedure. Determines the authorization protocols for each. The insurance authorization specialist is responsible for verifying patient eligibility, obtaining prior authorizations, and maintaining patient authorizations. Many of the low premium insurance covered patients suffer in the hands of the specialist’s ingenious ways to deny the permission for procedure. Knowledge of third party payer regulations including medicare, minnesota medical assistance, veterans affairs (va) and private insurance.

$16.00 to $16.00 hourly the robert half healthcare practice is. Research salary, company info, career paths, and top skills for insurance authorization specialist The insurance authorization specialist is responsible for selecting accurate medical records for patient safety and working with insurance companies and/or physician offices to complete insurance authorization requirements to secure payment. View the job description, responsibilities and qualifications for this position. A certificate program in medical coding and billing, a note on the costs of specialist visits, emergency situations, an insurance verification specialist with experience in hospital billing and more about insurance authorization specialist job.
 Source: qwikresume.com
Source: qwikresume.com
Apply to insurance verification specialist, prior authorization specialist, authorization specialist and more! 1,531 insurance authorization specialist jobs available on indeed.com. Insurance authorization specialist job description. They interview patients to assess their needs and work with insurance companies and. Obtains authorizations for surgical procedures, diagnostic testing, medications, outgoing referrals, and other services as part of daily operations.
 Source: uslegalforms.com
Source: uslegalforms.com
Knowledge of third party payer regulations including medicare, minnesota medical assistance, veterans affairs (va) and private insurance. Lehigh valley health network allentown, pa. The authorization specialist job role is to take insurance information from the clients and determine if any authorization is required for the service that is to be undertaken. Minimum of two years of experience in insurance authorization, billing, business administration. 10,148 medical insurance authorization specialist jobs available on indeed.com.
 Source: ziprecruiter.com
Source: ziprecruiter.com
Filter by location to see an insurance authorization specialist salaries in your area. Insurance authorization specialist responsibilities include: Apply for the job in insurance authorization specialist at ridgefield, ct. Job detailsjob type fulltimefull job descriptiondescription:providence stjoseph health is calling an insurance verification and authorization specialist work remotely within a 2 hour commute from portland, or.we are seeking an insurance verification and authorization specialist to be responsible for securing appropriate patient account reimbursement by. 1,496 insurance authorization specialist jobs available on indeed.com.
 Source: imbillionaire.net
Source: imbillionaire.net
The authorization specialist job role is to take insurance information from the clients and determine if any authorization is required for the service that is to be undertaken. Acquired insurance authorizations for procedures and tests ordered by the attending physician. Authorization specialists file documents and gather the required information for. An authorization specialist is responsible for reviewing insurance claims and determining the necessary settlement for the clients and involved parties. Obtains authorizations for surgical procedures, diagnostic testing, medications, outgoing referrals, and other services as part of daily operations.
 Source: qwikresume.com
Source: qwikresume.com
Serves as a patient advocate and functions as a liaison between the patient and payor to address reimbursement questions and avoid insurance delays. Job detailsjob type fulltimefull job descriptiondescription:providence stjoseph health is calling an insurance verification and authorization specialist work remotely within a 2 hour commute from portland, or.we are seeking an insurance verification and authorization specialist to be responsible for securing appropriate patient account reimbursement by. Minimum of two years of experience in insurance authorization, billing, business administration. Get more data about insurance authorization. The insurance authorization specialist is responsible for verifying patient eligibility, obtaining prior authorizations, and maintaining patient authorizations.
 Source: blog.accountmattersma.com
Coordinate completion of prior authorization, if needed; Job detailsjob type fulltimefull job descriptiondescription:providence stjoseph health is calling an insurance verification and authorization specialist work remotely within a 2 hour commute from portland, or.we are seeking an insurance verification and authorization specialist to be responsible for securing appropriate patient account reimbursement by. Serves as a patient advocate and functions as a liaison between the patient and payor to address reimbursement questions and avoid insurance delays. Apply for the job in insurance authorization specialist at ridgefield, ct. 1,496 insurance authorization specialist jobs available on indeed.com.
 Source: livecareer.com
Source: livecareer.com
$16.00 to $16.00 hourly the robert half healthcare practice is. The prior authorization specialists may become pharmacists with further education. Health care and home care experience preferred. Authorization specialists file documents and gather the required information for. Our company is looking for a insurance authorization specialist to join our team.
 Source: qwikresume.com
Source: qwikresume.com
Knowledge of medical terminology is. A certificate program in medical coding and billing, a note on the costs of specialist visits, emergency situations, an insurance verification specialist with experience in hospital billing and more about insurance authorization specialist job. 1,496 insurance authorization specialist jobs available on indeed.com. You will evaluate portions to be paid by the customer as well as perform all insurance related assignments as instructed. 1,531 insurance authorization specialist jobs available on indeed.com.
 Source: qwikresume.com
Source: qwikresume.com
The insurance authorization specialist is responsible for verifying patient eligibility, obtaining prior authorizations, and maintaining patient authorizations. Acquired insurance authorizations for procedures and tests ordered by the attending physician. Salaries estimates are based on 18 salaries submitted anonymously to glassdoor by an insurance authorization specialist employees. 1,531 insurance authorization specialist jobs available on indeed.com. The insurance authorization specialist is responsible for verifying patient eligibility, obtaining prior authorizations, and maintaining patient authorizations.
 Source: myperfectresume.com
Source: myperfectresume.com
Authorization specialists file documents and gather the required information for. A certificate program in medical coding and billing, a note on the costs of specialist visits, emergency situations, an insurance verification specialist with experience in hospital billing and more about insurance authorization specialist job. Knowledge of third party payer regulations including medicare, minnesota medical assistance, veterans affairs (va) and private insurance. Insurance authorization specialist job description template. Get more data about insurance authorization.

Our company is looking for a insurance authorization specialist to join our team. Obtaining detailed benefits for ordered test; $16.00 to $16.00 hourly the robert half healthcare practice is. They interview patients to assess their needs and work with insurance companies and. Salaries estimates are based on 18 salaries submitted anonymously to glassdoor by an insurance authorization specialist employees.
 Source: indotemplate123.com
Source: indotemplate123.com
Knowledge of third party payer regulations including medicare, minnesota medical assistance, veterans affairs (va) and private insurance. Research salary, company info, career paths, and top skills for insurance authorization specialist On average, insurance coordinators earn a difference of $1,494 lower per year. Serves as a patient advocate and functions as a liaison between the patient and payor to address reimbursement questions and avoid insurance delays. Obtaining detailed benefits for ordered test;
 Source: pdffiller.com
Source: pdffiller.com
Acquired insurance authorizations for procedures and tests ordered by the attending physician. View the job description, responsibilities and qualifications for this position. Get more data about insurance authorization. Filter by location to see an insurance authorization specialist salaries in your area. The authorization specialist job role is to take insurance information from the clients and determine if any authorization is required for the service that is to be undertaken.
 Source: qsstudy.com
Source: qsstudy.com
Knowledge of third party payer regulations including medicare, minnesota medical assistance, veterans affairs (va) and private insurance. Acquired insurance authorizations for procedures and tests ordered by the attending physician. 1,496 insurance authorization specialist jobs available on indeed.com. Research salary, company info, career paths, and top skills for insurance authorization specialist The insurance authorization specialist is responsible for verifying patient eligibility, obtaining prior authorizations, and maintaining patient authorizations.
This site is an open community for users to do submittion their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site serviceableness, please support us by sharing this posts to your favorite social media accounts like Facebook, Instagram and so on or you can also save this blog page with the title insurance authorization specialist by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.
